Between the global COVID-19 pandemic and the political environment, the past two years have been full of challenges. Nevertheless, every challenge brings an opportunity. In the case of the healthcare industry, that opportunity is leveraging our understanding of SDOH and finally pairing it with DE&I efforts to reduce health disparities.
What Do All These Letters Mean?
Unless you have been living under a rock, you have probably heard the terms “SDOH” and “DE&I”. But in case you have been living under a rock (and for the record, I don’t blame you, it’s been a crazy few years!), let’s quickly make sense of all these letters.
Social determinants of health, or SDOH, are conditions in which people are born, age, learn, worship, live, work, and play. These also include the wider set of forces and systems shaping the conditions of people’s daily lives. We typically categorize SDOH into five key areas:
- Education access and quality
- Economic stability
- Social and community context
- Neighborhood and built environment
- Healthcare access and quality
Though these are non-medical conditions, they have a tremendous impact on health outcomes.
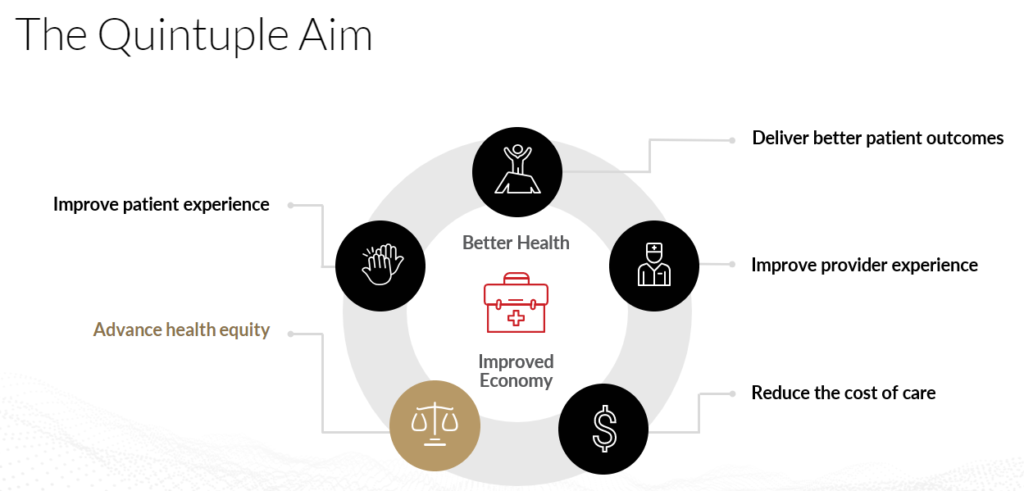
DE&I stands for diversity, equity, and inclusion. Diversity is the presence of differences within a given setting. Equity is the process of ensuring that processes and programs are impartial, fair and provide equal possible outcomes for every individual. Inclusion is the practice of ensuring that people feel a sense of belonging1. In the case of healthcare, addressing DE&I not only helps improve patient satisfaction and engagement and drive quality of care, it gets us closer to achieving the quintuple aim.
SDOH and DE&I can no longer be thought of independently if we are to reduce healthcare disparities.
READ MORE: Health Equity Trends: The Quintuple Aim
Health Disparities
Health disparities – inequities in the quality of health, healthcare, and health outcomes, are closely related to social or economic disadvantages. This topic has been getting a lot of attention from clinicians, policy makers, and the federal government in recent years. And rightfully so. Health disparities are expensive! They could cost the U.S. healthcare system approximately $320 billion. If not addressed, the cost of health disparities could reach $1 trillion or more by 20402.
Health disparities adversely affect groups of people who have systematically experienced greater obstacles to health based on racial background, ethnic background, or other characteristics linked to discrimination or exclusion3. Verywell Health provides some impactful examples4:
- Infant mortality: Babies born to Black women in the United States die at more than double the rate of babies born to white women.
- Dementia: Black people also have the highest risk for dementia, and are twice as likely to develop Alzheimer’s disease than white people in the United States.
- Cancer: People with lower incomes and education levels are more likely to get cancer and to die from it compared to their more affluent peers, and that gap appears to be widening.
- Obesity: Even after controlling for family income, rates of obesity in Black women and Mexican-American men are substantially higher than in other races or ethnic groups.
- Smoking: Native American/Alaska Native men and women have disproportionately higher rates of smoking, as do individuals who are unemployed or living below the federal poverty level.
EXPLORE NOW: Diversity, Equity & Inclusion in Healthcare
Impact of SDOH and DE&I on Health Disparities
There are many factors that contribute to the examples above and to health disparities in general, but none greater than SDOH. Communities of color, populations with a lower socioeconomic status, rural communities, people with cognitive and physical disabilities, and individuals who identify as LGBTQ+ are often disproportionately exposed to conditions and environments that negatively affect health risks and outcomes and lead to higher rates of health disparities5.
Social determinants of health determine approximately 80% of a person’s health status.
Therefore, it’s no surprise that healthcare organizations have been integrating SDOH into practice. More recently. they’re leveraging DE&I strategies to address equity to shift focus on access, affordability, and quality of care. But we cannot allow these efforts to be siloed if we are to move the needle on reducing health disparities.
Combining DE&I strategies with SDOH efforts can have a profound impact on the delivery of care and clinical outcomes. As providers recognize the need for diversity and inclusion within the healthcare system, greater steps to address equity and access within practices are forcing them to look at key healthcare indicators through a SDOH lens. By doing so, providers can meet the patient where they are in the healthcare journey.
Understanding their unique needs and challenges – regarding clinical and nonclinical factors not previously considered – is vital to designing a suitable and sustainable treatment plan. For example, knowing a patient does not have consistent access to transportation would allow the provider to offer up alternative options closer to the patient’s home, virtual health visits, or a free transportation service provided by the health system/clinic or community programs.
To ensure, SDOH and other relevant, non-clinical data is available, healthcare organizations need to increase collaboration with their communities and invest in tools and technologies to allow for this data and information to be readily available.
For instance, the use of artificial intelligence (AI) and natural language processing (NLP) to scan through clinical notes and data to identify SDOH is not only efficient, but highly valuable. Healthcare does not exist in a vacuum. Identifying the challenges while offering personalized health support will go a long way in closing the gap on health disparities.
LEARN MORE: 5 Commonly Asked Questions About Intrinsic Bias in AI/ML Models in Healthcare
What Else Can We Do?
The growing need to address SDOH and DE&I to reduce health disparities can no longer simply be acknowledged as something that needs to be done. We actually need to do something!
Despite the increased recognition of SDOH and DE&I and its impact on health disparities, minimal agreement on how to address the issue exists. According to KKF, assuring greater equity and accountability of the healthcare system is important to a growing constituency base of health plan purchasers, payers, and providers and speaks to four areas where we can begin to address health disparity concerns6:
- Raising public and provider awareness of racial/ethnic disparities in care: Perceptions of a problem often influence the actions taken (or not taken) to change policy and practices. If the public or providers are unaware that a problem exists or misunderstands the nature of the problem, it can be difficult to direct resources to address that problem. We need greater efforts to raise the public’s awareness of racial/ethnic healthcare disparities.
- Expanding health insurance coverage: Health insurance impacts when people get necessary medical care, where they receive care, and how healthy people are. Compared with the insured, the uninsured are less likely to have a regular doctor or to get timely and routine care. They are also more likely to be hospitalized for preventable conditions. Minority Americans are much less likely to be ensured, even after accounting for work status.
- Improving the capacity and number of providers in underserved communities: Since the 1970s, there have been efforts to increase the number of health professionals in medically underserved areas. Despite this, members of racial/ethnic minority groups are still underrepresented in the healthcare workforce and are more likely to live in neighborhoods that lack adequate health resources. This leads to an increased use of emergency care as the primary source of care, rather than a primary care doctor who can provide patient-centered care. This is a result of many factors, including the higher likelihood of being uninsured and the limited availability of primary care physicians in some communities of color.
- Increasing the knowledge base on causes and interventions to reduce disparities: Although evidence of healthcare disparities is substantial, the evidence-base for developing interventions to eliminate these disparities remains limited. There are growing efforts, such as SDOH, to address factors outside the healthcare system. In addition, DE&I efforts to examine how to train healthcare providers to a) offer culturally and linguistically appropriate services, b) increase the use of electronic medical records to decrease medical errors and improve coordination of care, and c) increase the use of financial incentives to promote high quality healthcare may serve as ways to reduce health disparities. Increasing the knowledge base will require investing in routinely collecting and analyzing healthcare data across racial/ethnic groups and funding to support data collection.
If we are truly to make an impact, we need to shift from being reactive to being proactive. We must deliver healthcare that is equitable, inclusive, and reduces health inequities by addressing SDOH and leveraging the efforts around DE&I. Care goes far beyond the four walls of a hospital or clinic, and everyone deserves access to quality care!
References:
- https://builtin.com/diversity-inclusion/what-does-dei-mean-in-the-workplace
- https://www.forbes.com/sites/debgordon/2022/06/23/health-inequities-could-cost-the-us-health-system-1-trillion-by-2040-new-report-says/?sh=24f689741ba9
- https://www.ahajournals.org/doi/10.1161/CIR.0000000000000936
- https://www.verywellhealth.com/health-disparities-4173220
- https://www.ncsl.org/research/health/health-disparities-overview.aspx
- https://www.kff.org/racial-equity-and-health-policy/issue-brief/eliminating-racialethnic-disparities-in-health-care-what/





Thank you for sharing Health Disparities: Addressing Care Beyond the Four Walls.